Expo
view channel
view channel
view channel
view channel
Medical Imaging
AICritical Care
Patient CareHealth ITPoint of CareBusiness
Events
Webinars

- Glowing Bacterial Sensors Could Improve Detection of Gut Illness
- Gut Bacteria from Amphibians and Reptiles Show Complete Tumor Elimination
- Innovative ‘Poop Pills’ Dramatically Improve Cancer Treatment
- High-Dose Inhaled Nitric Oxide Emerges as Promising Antimicrobial Therapy
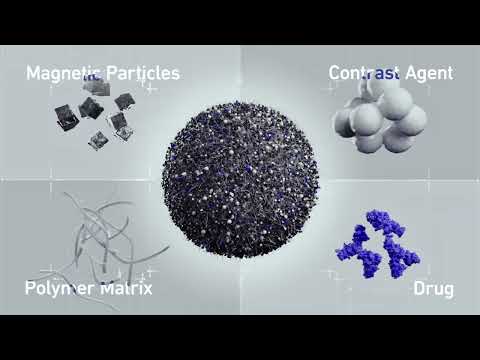
- New Nanomaterial Kills Cancer Cells While Sparring Healthy Tissues
- Boengineered Tissue Offers New Hope for Secondary Lymphedema Treatment
- New AI Approach to Improve Surgical Imaging
- Dual-Energy Catheter Brings New Flexibility to AFib Ablation
- 3D Bioprinting Pushes Boundaries in Quest for Custom Livers
- First-Of-Its-Kind Probe Monitors Fetal Health in Utero During Surgery
- VR Training Tool Combats Contamination of Portable Medical Equipment
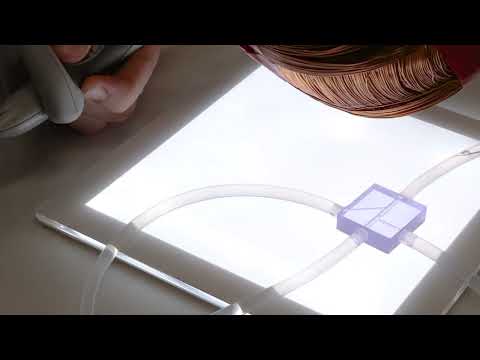
- Portable Biosensor Platform to Reduce Hospital-Acquired Infections
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
- WHX in Dubai (formerly Arab Health) to debut specialised Biotech & Life Sciences Zone as sector growth accelerates globally
- WHX in Dubai (formerly Arab Health) to bring together key UAE government entities during the groundbreaking 2026 edition
- Interoperability Push Fuels Surge in Healthcare IT Market
- Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies

 Expo
Expo
- Glowing Bacterial Sensors Could Improve Detection of Gut Illness
- Gut Bacteria from Amphibians and Reptiles Show Complete Tumor Elimination
- Innovative ‘Poop Pills’ Dramatically Improve Cancer Treatment
- High-Dose Inhaled Nitric Oxide Emerges as Promising Antimicrobial Therapy
- New Nanomaterial Kills Cancer Cells While Sparring Healthy Tissues
- Boengineered Tissue Offers New Hope for Secondary Lymphedema Treatment
- New AI Approach to Improve Surgical Imaging
- Dual-Energy Catheter Brings New Flexibility to AFib Ablation
- 3D Bioprinting Pushes Boundaries in Quest for Custom Livers
- First-Of-Its-Kind Probe Monitors Fetal Health in Utero During Surgery
- VR Training Tool Combats Contamination of Portable Medical Equipment
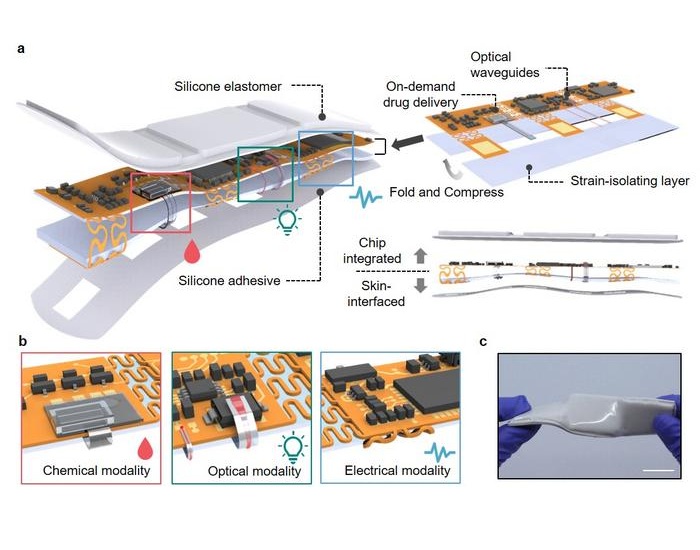
- Portable Biosensor Platform to Reduce Hospital-Acquired Infections
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
- WHX in Dubai (formerly Arab Health) to debut specialised Biotech & Life Sciences Zone as sector growth accelerates globally
- WHX in Dubai (formerly Arab Health) to bring together key UAE government entities during the groundbreaking 2026 edition
- Interoperability Push Fuels Surge in Healthcare IT Market
- Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies