Expo
view channel
view channel
view channel
view channel
Medical Imaging
AICritical CareSurgical Techniques
Health ITPoint of CareBusiness
Events
Webinars

- AI Model Accurately Predicts Neurological Recovery After Cardiac Arrest
- Battery-Free Nano-Sensors Pave Way for Next-Generation Wearables
- Imaging Technology Detects Early Signs of Cardiovascular Risk Through Skin
- New Therapeutic Approach Marks Breakthrough in Pediatric Heart Disease
- AI Model Accurately Identifies Prediabetics Using Only ECG Data
- Dual-Energy Catheter Brings New Flexibility to AFib Ablation
- 3D Bioprinting Pushes Boundaries in Quest for Custom Livers
- First-Of-Its-Kind Probe Monitors Fetal Health in Utero During Surgery
- Light-Activated Tissue Adhesive Patch Achieves Rapid and Watertight Neurosurgical Sealing
- Ultrasound Device Offers Non-Invasive Treatment for Kidney Stones
- VR Training Tool Combats Contamination of Portable Medical Equipment
- Portable Biosensor Platform to Reduce Hospital-Acquired Infections
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
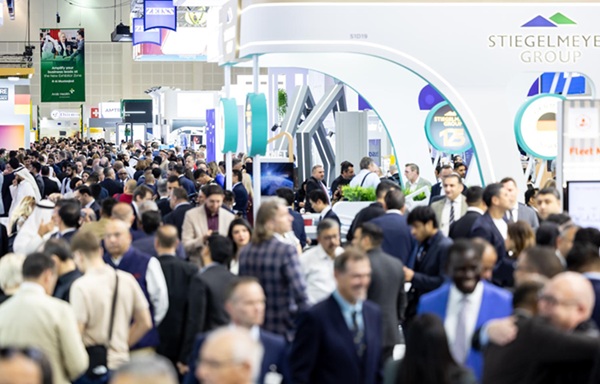
- WHX in Dubai (formerly Arab Health) to bring together key UAE government entities during the groundbreaking 2026 edition
- Interoperability Push Fuels Surge in Healthcare IT Market
- Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
- B. Braun Acquires Digital Microsurgery Company True Digital Surgery
- CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry

 Expo
Expo
- AI Model Accurately Predicts Neurological Recovery After Cardiac Arrest
- Battery-Free Nano-Sensors Pave Way for Next-Generation Wearables
- Imaging Technology Detects Early Signs of Cardiovascular Risk Through Skin
- New Therapeutic Approach Marks Breakthrough in Pediatric Heart Disease
- AI Model Accurately Identifies Prediabetics Using Only ECG Data
- Dual-Energy Catheter Brings New Flexibility to AFib Ablation
- 3D Bioprinting Pushes Boundaries in Quest for Custom Livers
- First-Of-Its-Kind Probe Monitors Fetal Health in Utero During Surgery
- Light-Activated Tissue Adhesive Patch Achieves Rapid and Watertight Neurosurgical Sealing
- Ultrasound Device Offers Non-Invasive Treatment for Kidney Stones
- VR Training Tool Combats Contamination of Portable Medical Equipment
- Portable Biosensor Platform to Reduce Hospital-Acquired Infections
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- WHX in Dubai (formerly Arab Health) to bring together key UAE government entities during the groundbreaking 2026 edition
- Interoperability Push Fuels Surge in Healthcare IT Market
- Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
- B. Braun Acquires Digital Microsurgery Company True Digital Surgery
- CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry